Written by Vicki McLellan
Self-destructive behaviours like self-harm, disordered eating and substance misuse naturally spark concern in loved ones and care providers.
The risks and consequences of such behaviours can be far reaching. It makes sense then that motivation most often lies in ‘fixing’ the behaviour and eliminating the risks.
Frequently, the question posed is ‘Why the behaviour?’. However, as suggested by Dr Gabor Mate, perhaps the more pressing question is ‘Why the pain?’ (2018).
Self-destructive behaviour is an often misunderstood issue that profoundly impacts both the individual and those close to them. Where current standard treatment approaches focus on thought and behaviour patterns in the ‘here and now’, there is growing evidence to support therapeutic interventions which explore the root causes of the behaviours.
Renowned trauma specialist, Dr Janina Fisher explains that each incident of destructive behaviour results in short term relief from psychological pain, followed by a ‘rebound effect’ which may include negative social consequences, traumatic exposure or reinforcing experiences. This increases the likelihood that the same destructive behaviours will be stimulated again (2024).

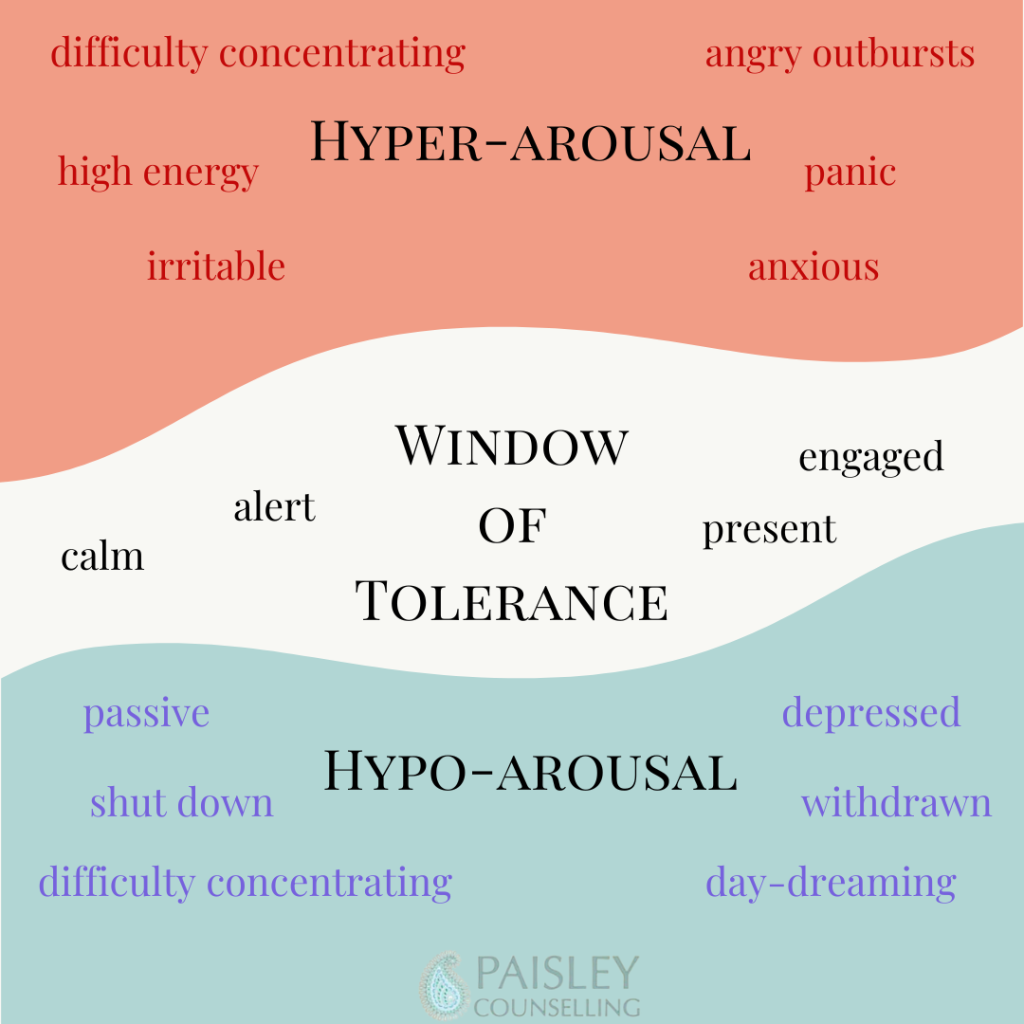
Consultant Psychiatrist, Dr Frank Corrigan explains that destructive behaviours are an attempt to regulate a dysregulated nervous system (2010). A cycle of re-traumatising self-destructive responses is set in motion and since the individual likely develops a tolerance to the addictive behaviour, increased or more intense attempts to self-regulate are needed to achieve some relief.
Dr Janina Fisher explains that, despite the best efforts of health professionals, successful treatment of destructive coping behaviours is extremely challenging because the fear of their underlying pain is much greater than the fear of the risks involved in their behaviours (2024).
Self-destructive behaviours are self-protective strategies offering a sense of safety and a way to cope and regulate through deep, often unconscious pain.
Although challenging thought and behaviour patterns is one aspect of successful therapy, it is not enough.
I believe that much of the work is possible only as a stable therapeutic relationship begins to be established. It is important to find a counsellor who feels like a ‘good fit’ for you. Who can sit with you in your pain and honour the protections that have helped you survive whilst offering safety, compassion and care. In this way, you can work together to uncover the underlying thread of pain, processing and establishing a new level of safety within and finding new, safer ways to regulate your system.
References
Corrigan, F. F. J. N. D. (2010). Autonomic dysregulation and the Window of Tolerance model of the effects of complex emotional trauma. Journal of Psychopharmacology, 0(0), pp. 1-9.
Fisher, D. J. (2024). Understanding Self Destruction. s.l.:Dr Janina Fisher Ph.D. for Instagram and Facebook.
Mate, G. (2018). In the Realm of Hungry Ghosts. London: Vermillion.